Accounts receivable management is the ability of keeping record of how much praise the company has given its consumers, and when the company can anticipate it back. Usually these engage an amount that a consumer owes to the company concerning the trade of any product or service. Doctors afford patients with the best care probable and are expecting to be paid for their services from the Assurance Company and patients. The healthcare assurance system works in an inquisitive way where the provider delivers service and is re-imbursed at a much later phase.
 Whether we like it or not, the assurance model is now to stay and it is very important for both small providers like doctors’ offices and general practitioner groups and large providers like big medical clinics to industriously follow up on payments that are unpaid. The accounts receivable management has developed in to the most noteworthy section in these organizations as they help out in recovering the money from patients and assurance companies and help out to keep the business successively.
Whether we like it or not, the assurance model is now to stay and it is very important for both small providers like doctors’ offices and general practitioner groups and large providers like big medical clinics to industriously follow up on payments that are unpaid. The accounts receivable management has developed in to the most noteworthy section in these organizations as they help out in recovering the money from patients and assurance companies and help out to keep the business successively.
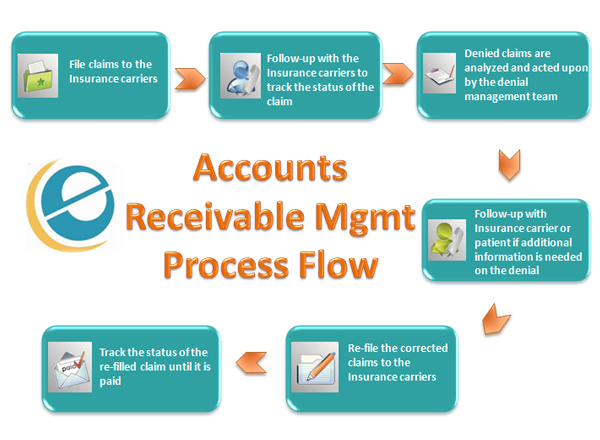
The task of accounts receivable management has evolved from a mere departmental movement to a specialized skill midpoint by itself and requires professionals so that doctor’s office can focus on delivering the best concern to their patients. This action has become a significant and essential part of the overall billing services that are offered by medical billing companies. The procedure of entering the charge codes into the healthcare claim sheet is called charge entry. There are precise rules defined by the assurance companies on what constitutes a valid claim and there are hundreds of rules some easy and others multifaceted to determine the validity of a claim. This is a very important step as this considerably lowers the risk of claim denials. The claims are then submitted to the assurance company for processing. The assurance company processes the claim and sends a payment remittance to the billing company but the reply time is unpredictable and hence the requirement of an exclusive accounts receivable team. The Account Receivable squad takes over the claim and follows up with the insurance company for payments.
The Account Receivable squad analyzes the claim for denials, partial expenses and non-payments and if the claim has been filed wrongly, the claim is corrected and re-submitted. The Billing Account Receivable Management team develops a stable contact method with the assurance company, patient and the medical administrative center and carefully follows up to make sure quick and complete expense. The skill sets and qualities expected from members of the accounts receivable management team are good diagnostic skills, concentration to detail, carefulness and above all, patience. Squad members with these qualities are expensive assets to the association and will make sure that the medical office receives their payments promptly.



